Understand Your Gut Microbiome with the Experts in GA
What are Microbiome and Probiotics?
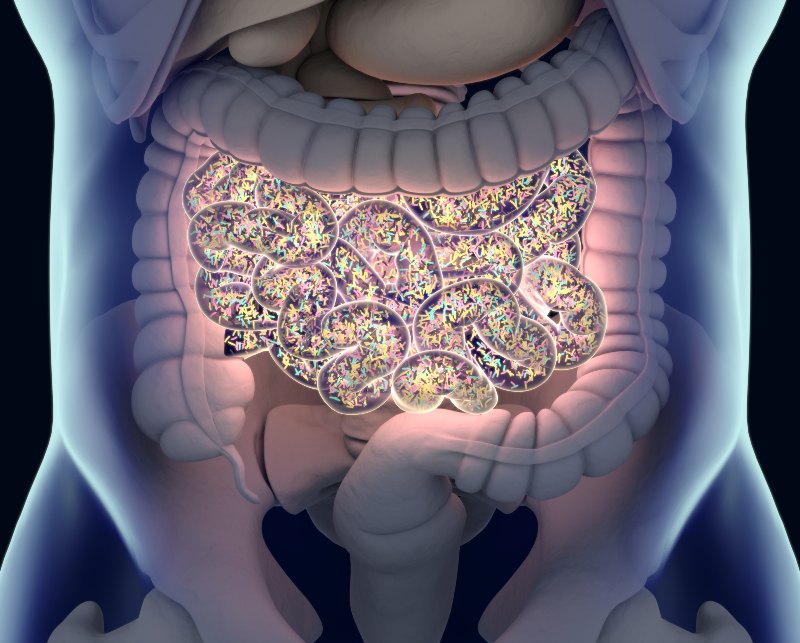
The microbiome refers to trillions of microorganisms residing in your gut, including bacteria, viruses, fungi, and other microbes. This diverse ecosystem plays a pivotal role in your overall health, influencing digestion, immunity, and even mental well-being.
Probiotics, on the other hand, are live beneficial bacteria or yeasts that you can consume through certain foods and supplements. These friendly bacteria are essential in supporting a balanced gut microbiome. Probiotics offer numerous benefits for digestive health and the rest of your body.
The Role of the Microbiome
Your gut microbiome is an incredibly dynamic environment that influences your digestive health significantly. It helps break down food, absorb nutrients, and produce essential vitamins. A healthy microbiome acts as a barrier against harmful bacteria and pathogens, reducing the risk of infections. It also communicates with the immune system, ensuring your body responds appropriately to potential threats.
Disruptions to the microbiome can lead to gut microbiome diseases such as inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), and other digestive issues. Therefore, understanding what gut microbiome is and maintaining its balance is vital for good health. Our GI services can help you with this.
Benefits of Probiotics
Probiotics offer many health benefits by enhancing the composition of your gut microbiome. Some key probiotic health benefits include:
- Improved Digestion – Probiotics aid in breaking down food more efficiently, alleviating symptoms like bloating and constipation.
- Enhanced Immune Function – By promoting the growth of beneficial bacteria, probiotics support your immune system's ability to fight infections.
- Alleviation of GI Disorders – Studies have shown that probiotics can help manage symptoms of IBS and reduce the severity of IBD flare-ups.
- Better Mental Health – The gut-brain axis indicates that a healthy gut microbiome can positively impact mood and cognitive functions.
Sources of Probiotics
Probiotics can be found in various foods and supplements. Fermented foods are particularly rich in these beneficial bacteria. Some excellent sources include:
- Yogurt – A well-known probiotic-rich food that can improve gut health.
- Kefir – A fermented milk drink packed with diverse probiotic strains.
- Sauerkraut and Kimchi – Fermented vegetables that offer a robust mix of probiotics and fiber.
- Miso and Tempeh – Fermented soy products that are not only rich in probiotics but also protein.
- Probiotic Supplements – Available in pill, powder, or liquid form, these supplements provide concentrated doses of beneficial bacteria.
How to Maintain a Healthy Microbiome
- Eat a Diverse Diet – Consuming a variety of fruits, vegetables, and whole grains ensures a wide range of nutrients that promote a healthy microbiome.
- Limit Antibiotics – While necessary at times, antibiotics can disrupt the balance of your gut bacteria, so they should be used judiciously.
- Stay Active – Regular physical activity can positively affect gut microbiome diversity.
- Manage Stress – Chronic stress can negatively impact your gut health, so incorporating stress-reducing activities can be beneficial.
- Stay Hydrated – Drinking plenty of water supports the mucosal lining of the intestines, promoting a healthy microbiome.
Why Choose GI Specialists of Georgia?
Contact Us Today in Atlanta, GA
If you are interested in learning more about how the gut microbiome and probiotics can benefit your digestive health, or if you're seeking effective gut microbiome disease treatment, reach out to GI Specialists of Georgia. Our experienced team is ready to guide you on your journey to better health.
Don't wait to take charge of your digestive health. Contact us today to schedule a consultation and discover how we can support your gut health, digestion & microbiome support needs. Your well-being is our priority, and we are dedicated to helping you achieve optimal digestive health.
Explore our services and take the first step toward a healthier you.
What is Barrett’s Esophagus?
Learn More about Barrett’s Esophagus
A long-standing history of gastroesophageal reflux disease (GERD), also called heart burn or acid reflux is the primary reason for developing BE. About 10% of patients with GERD develop BE.
Primarily BE is seen in Caucasian male patients, obese, ages > 50 with chronic complaints of GERD. About less than 1% of the patients with BE can develop esophageal adenocarcinoma (food pipe cancer) which is potentially fatal.
There are no specific symptoms for BE. Symptoms are often related to the presence of GERD. Some patients with Barrett’s Esophagus may have silent GERD (without symptoms of acid reflux or heartburn).
However, as mentioned above, Caucasian male patients, obese, ages > 50 with chronic complaints of GERD are at a higher risk of developing BE and thereby more at a risk for BE related esophageal adenocarcinoma (BEAC). However, any patient can develop this condition if they have long-standing GERD symptoms.
Patients diagnosed with BE are at an increased risk for developing esophageal adenocarcinoma. About less than 1% of patient with BE develop adenocarcinoma. Usually, the process of developing adenocarcinoma from BE involves the stage of dysplasia (pre-malignant changes) which include low-grade dysplasia and high-grade dysplasia and then cancer.
BE →← Low-Grade Dysplasia →← High-Grade Dysplasia → Adenocarcinoma
Hence patients are continued on acid reflux medications (proton-pump inhibitors) and they undergo periodic surveillance of upper endoscopies with biopsies to detect the changes of dysplasia.
Primarily the goal of treatment should include strictly controlling the stomach acid production and thereby symptoms of GERD.
Lifestyle changes include:
- Weight loss
- Diet changes: avoiding alcohol, tobacco, and caffeinated drinks
- Sleeping with the head of the bed elevated and not lying down for 3 hours after eating.
Medications, which control acid production, include proton-pump inhibitors, antacids, H2 blockers and promotility agents. Medications help in decreasing the acid production and thereby decreasing acid exposure of the lining of the lower esophagus and thereby decreasing the incidence of BE. Medications are also primarily used even after developing low-grade dysplasia.
There are definitive therapies once high-grade dysplasia ensues. These include
- Radiofrequency ablation (RFA), which uses radio waves delivered through an endoscope to destroy abnormal cells.
- Endoscopic spray cryotherapy, which applies cold nitrogen or carbon dioxide gas through an endoscope to freeze and destroy the abnormal cells.
- Endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD) is an endoscopic surgery wherein the abnormal lining of the cells are lifted off the wall and cut off via the endoscope.
- Finally, surgery to remove the lower part of the esophagus in early cancers.
Schedule an Appointment with Our Atlanta-Area Gastroenterologists
"*" indicates required fields

